Nerve pain, often described as a burning or electric shock-like sensation, can be particularly distressing when it flares up during the night. Many individuals suffering from conditions like peripheral neuropathy or https://postheaven.net/calirawfostrelgwkv/nerve-pain-vs-muscle-pain-understanding-the-key-differences sciatica report that their discomfort intensifies as they settle into bed. This phenomenon raises important questions about the nature of nerve pain and what factors contribute to its nighttime exacerbation.
Understanding why nerve pain worsens at night is essential for effective management and treatment. The interplay of physiological, psychological, and environmental factors creates a perfect storm that can leave sufferers tossing and turning, desperate for relief.
The Nature of Nerve Pain
Nerve pain, or neuropathic pain, arises from damage to or dysfunction of the nervous system. Unlike typical muscle or joint pain caused by injury or inflammation, nerve pain originates in the damaged nerves themselves. This can manifest in various ways – from tingling sensations and numbness to sharp, stabbing pains.
People with conditions such as diabetes may experience diabetic neuropathy, which leads to nerve damage over time. Similarly, those who have had shingles can develop postherpetic neuralgia, where nerve endings remain sensitized long after the rash has healed. The symptoms are often unpredictable and can vary significantly between individuals.
Common Symptoms of Nerve Pain
Individuals experiencing nerve pain may report:
- Burning sensations: A hot feeling in the affected area. Tingling or "pins and needles": Often felt in extremities like hands and feet. Sharp shooting pains: Sudden bursts of intense discomfort. Numbness: Reduced sensation in affected areas.
These symptoms can fluctuate throughout the day but are notably more pronounced during nighttime hours.
Factors Contributing to Nighttime Nerve Pain
Several factors contribute to why nerve pain may intensify at night. Understanding these can help patients manage their symptoms more effectively.
1. Body Position
The position in which one sleeps plays a crucial role in how nerves are compressed or stretched during rest. For instance, lying on one's side may put pressure on certain nerves in the arms or legs, leading to increased discomfort. Additionally, certain sleeping positions might exacerbate conditions like sciatica if the sciatic nerve is irritated during sleep.
2. Reduced Distractions
During the day, various activities distract from discomfort; however, at night there is less sensory input to mask the pain. The quiet environment allows individuals to become hyper-aware of their bodies and any present discomforts. This heightened awareness can amplify feelings of pain that might have been overlooked during busier hours.
3. Hormonal Changes
Circadian rhythms affect hormone levels throughout the day and night cycle. Hormones like cortisol tend to decrease at night while melatonin levels rise; this transition influences how we perceive and respond to pain signals. Consequently, individuals may experience an increase in sensitivity to pain during nighttime hours due to these hormonal shifts.
4. Temperature Sensitivity
Many people find that their nerve pain worsens with changes in temperature. Cold nights can exacerbate symptoms due to reduced blood flow to extremities; cold temperatures may increase sensitivity around already compromised nerves. Conversely, heat may temporarily alleviate some symptoms but could also lead to a perception of increased discomfort when it dissipates.
5. Psychological Factors
Stress and anxiety often escalate at night when individuals reflect on their day’s events or worry about upcoming tasks. This mental strain can heighten awareness of physical discomforts including nerve pain due to its strong connection with psychological health.
Managing Nighttime Nerve Pain
While understanding these contributing factors is helpful for managing nighttime flare-ups of nerve pain, it is equally important to explore treatment options tailored specifically for nighttime relief.
Medications
Certain medications may help alleviate nerve pain specifically when taken before bed:
- Gabapentin: Often prescribed for neuropathic pain relief. Pregabalin (Lyrica): Another common choice for managing chronic nerve-related discomfort. Duloxetine (Cymbalta): An antidepressant that has proven effective for some types of neuropathic pain.
Consulting with a healthcare provider about timing doses appropriately can make a significant difference in managing symptoms effectively through the night.
Lifestyle Adjustments
Making small adjustments to daily habits can also play a vital role in symptom management:
- Sleep Hygiene: Establishing a calming bedtime routine helps signal your body that it's time for rest. Optimal Sleep Positioning: Using supportive pillows can alleviate pressure on nerves by helping maintain proper alignment.
For example, placing a pillow between your knees while lying on your side could relieve pressure on your lower back nerves while you sleep.
Natural Remedies
Many find relief through natural remedies such as:
- Essential Oils: Oils like lavender possess calming properties; diffusing them before bed may promote relaxation. Herbal Supplements: Certain supplements such as alpha-lipoic acid have shown promise in alleviating diabetic neuropathy symptoms.
Be sure always to consult healthcare providers before beginning new supplements or herbal treatments—especially if other medications are involved—to avoid potential interactions.
The Role of Diet
Dietary choices also influence overall nerve health and function:
- Antioxidant-rich Foods: Including fruits and vegetables high in antioxidants helps combat oxidative stress on nerves. Healthy Fats: Omega-3 fatty acids found in fish oil support neurological health by reducing inflammation.
Incorporating foods rich in B vitamins—like whole grains and leafy greens—may promote better nerve function as well.
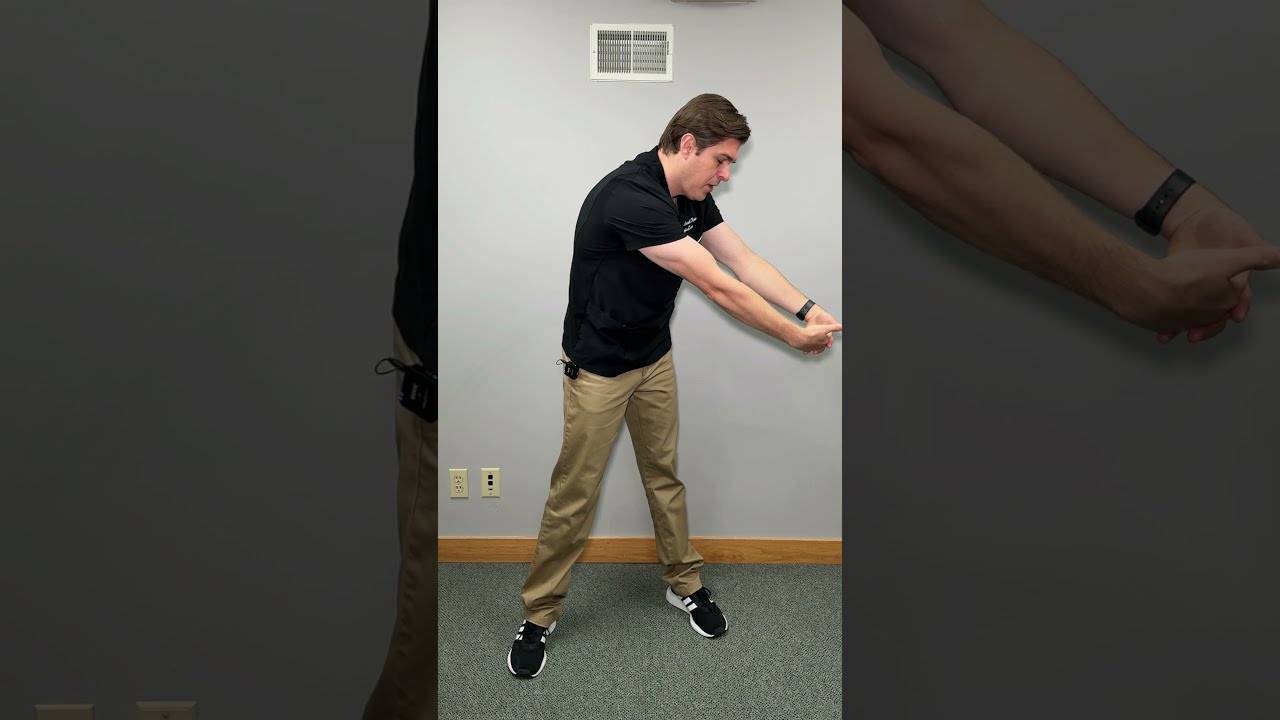
Exercises for Nerve Health
Gentle exercises help improve circulation while reducing tension around sensitive nerves:
Stretching: Gentle stretches targeting affected areas reduce stiffness and improve flexibility. Walking: Regular walks encourage blood flow without excessive strain on joints or nerves. Yoga/Pilates: These practices focus on mindful movement and breathing techniques that ease muscle tension while promoting relaxation.Always start slowly with any exercise regimen focusing first on gentle movements before gradually increasing intensity based on comfort levels.
When Is It Time To Seek Help?
If nighttime nerve pain becomes unbearable or disrupts sleep consistently despite home remedies or lifestyle changes, consulting with healthcare professionals is vital for evaluating underlying conditions that could require specific interventions—such as physical therapy or interventional procedures designed explicitly for targeted relief strategies based upon individual needs!
Finding effective ways through medical guidance allows not only improved management but promotes overall quality-of-life enhancements amidst ongoing challenges posed by chronic illnesses affecting neurological systems!
By addressing both physical symptoms through appropriate therapies alongside emotional resilience-building practices—from mindfulness techniques down through social supports available within communities—we equip ourselves toward navigating complexities presented by persistent health concerns together!